Vitamin D
Vitamin D Deficiency
Definition / Description
Vitamin D deficiency is a major public health problem worldwide in all age groups causing adverse effects on skeletal health and other health consequences.
Vitamin D regulates and modulates the physiology and function of multiple human systems, including the skeletal muscle. It is a necessary vitamin for calcium absorption, maintaining serum calcium and phosphate concentrations to enable normal mineralization of bone, and to prevent hypocalcemic tetany. It is also needed for bone growth and bone remodelling by osteoblasts and osteoclasts.
Inadequate amounts of vitamin D is most commonly associated with rickets in children and osteomalacia in adults, where bones soften and loose integrity. Serum levels less than 20 mg/mL are considered deficient.
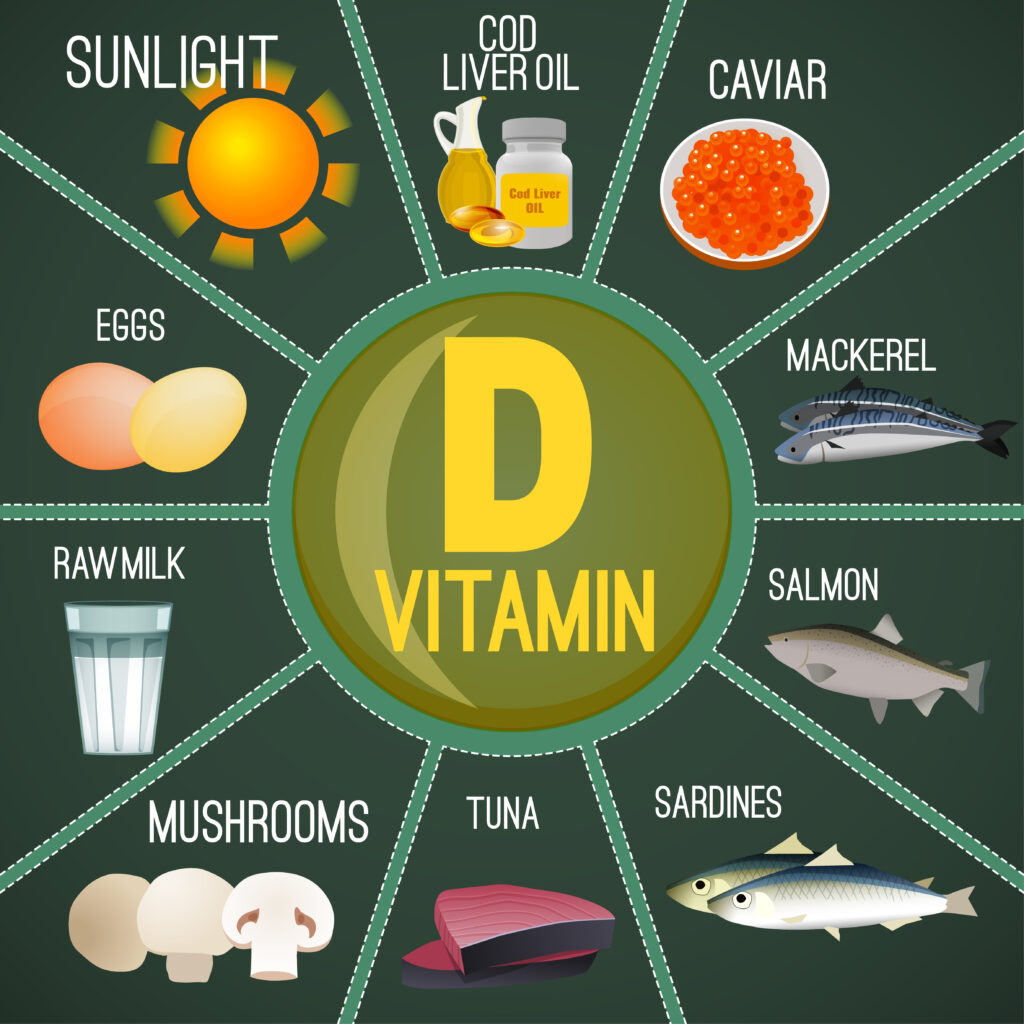
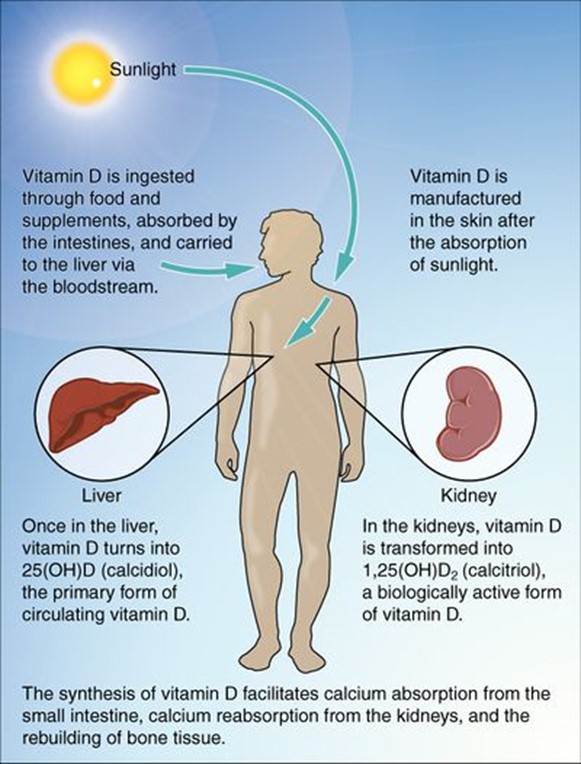
Vitamin D, also known as calcidiol or 25(OH)D, is a fat-soluble vitamin obtained from sun exposure, food, and supplements. It is not naturally present in many foods but is often used to fortify food or taken as a dietary supplement. Vitamin D is synthesized in the body when cholesterol (7-dehydrocholesterol) activates with UVB rays from sunlight. When ingested, the intestines absorb the vitamin and send it to the liver and kidneys for further processing.
Risk Factors
- Geriatric population
- Infants
- People with limited sun exposure
- Fat malabsorption
- Obesity (all ages): fat soluble vitamin is easily stored in adipose tissues –> decrease vitamin D in bloodstream
- Gestational diabetes
- Poor general health status
- Hypertension
- Insufficient daily intake of milk or other vitamin D containing foods
- Depression
- Burn patients
- Living in polluted climates
Possible causes: northern countries have little exposure to sunlight; clothing covering major surfaces of the body year-round such as with Arab women.
Characteristics / Clinical Presentation
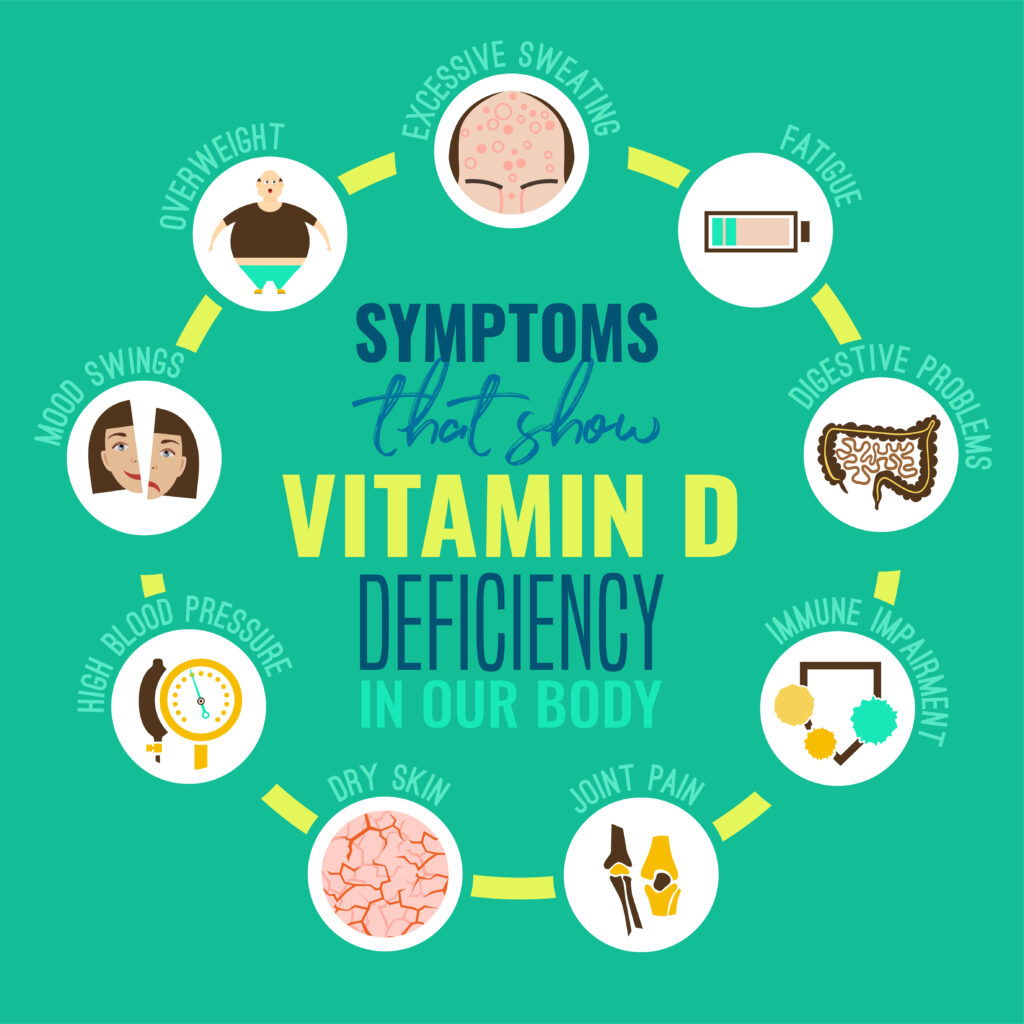
Adults generally present with the diagnosis of osteomalacia, which may include the following signs and symptoms:
- General muscle weakness
- Falls
- Fractures
- Severe bone pain
- Myalgia
- Decreased functional status
- Decreased progress during rehabilitation
- Fatigue
- Depression
Children typically present with rickets as their diagnosis, which may include the following signs and symptoms:
- Bowing of the long bones
- Widening, fraying, and clubbing in areas of active bone growth, predominantly around the metaphyseal ends of the long bones and sternal ends of the ribs.
Associated Co-morbidities
Osteoporosis
The hormone 7-dehydrocholesterol decreases in the skin as a person ages. By age 65, approximately only 25% of it remains in the body, leading to decreased synthesis of vitamin D and therefore calcium absorption.
Skeletal Deformities
In children with rickets there is often bowing of the long bones and widening, fraying, and clubbing near epiphyseal (growth) plates. Predominant areas include metaphysis of the long bones and sterna ends of the ribs, which is also known as rachitic rosary.
Electrolyte Imbalance
Often associated with hypomagnesemia.
Hyperparathyroidism
Parathyroid hormone (PTH) is a key hormone that regulates renal synthesis of calcidiol or 25(OH)D, which therefore maintains calcium ions in the blood. Low levels of vitamin D (calcidiol) and calcium ions in the blood stimulate the PTH. Through this mechanism, the active vitamin D metabolite [1,25(OH)2D], also known as calcitriol, promotes calcium supply to the bloodstream. As the cascade progresses, parathyroid is overstimulated, causing secondary hyperparathyroidism.
Cancer
Vitamin D may play a role in the prevention of colon, prostate, and breast cancers. Due to vitamin D receptors’ presence in colon, prostate, and breast tissues, vitamin D receptors often play a role in the proliferation of cells and their response to various stimuli. The lack therefore may indicate possible increase of cancer risk.
Myofascial Trigger Points / Myalgia
Other potential comorbidities
Diabetes (type I and II), Insulin Intolerance, Hypertension, Multiple Sclerosis (MS), and decreased cognition as seen in Alzheimer’s disease.
Medications That Prevent Vitamin D Absorption
- Anticonvulsants: (phenytoin, carbamazepine, Phenobarbital)
- Thiazide diuretics
- Corticosteroids
- Nicotine
- Cholesterol-lowering medications: (Cholestyramine, colestipol, ezetimibe)
- Cimetidine
- Heparin
- Diet agents (xenical, Alli)
Etiology / Causes
Adults
Primary causes include: inadequate sun exposure, insufficient supplementation, pregnant/lactating, and obesity.
Children and adolescents
Main causes include: inadequate sun exposure, inadequate vitamin supplementation, and breastfeeding without vitamin D supplementation.
Other causes
- Low intake of vitamin D in diet
- Poor renal function: reduces conversion of 25(OH)D to active metabolite in kidney
- Intestinal malabsorption problems, often associated with ageing ; irritable Bowel Syndrome (IBS)
- Long-term uses of anticonvulsants, which accelerates breakdown of the active forms of vitamin D
- Autoimmune disorders
Systemic Involvement
- Musculoskeletal System: Severe vitamin D deficiency may be associated with non-specific musculoskeletal pain, causing bone, muscle, and/or joint pain. Vitamin D affects muscle function and structure and vitamin D deficiency causes muscle weakness.
- Endocrine System: Secondary hyperparathyroidism.
- Cardiovascular System: Research suggests that low vitamin D may be a risk factor for certain arterial diseases such as Peripheral Artery Disease, Congestive Heart Failure, and Aortic Aneurysms. It may also contribute to decreased protection over lung function and increase lung functional decline in smokers. Vitamin D may have an affect on cardiac contractility, vascular tone, and cardiac tissue maturation due to the vitamin D receptors on the heart muscle. Therefore, vitamin D may play a role in the pathogenesis of CV problems.
- Gastrointestinal: Due to vitamin D receptors’ presence in colon tissues, vitamin D receptors play a role in the proliferation of cells and their response to stimuli. Therefore, a deficiency in vitamin D may play a role in colon cancer. Also as mentioned before, there is a lack of suppression of autoimmune diseases, such as Irritable Bowel Syndrome (IBS) when a vitamin D deficiency is present.
- Psychosocial System: Low levels of vitamin D are associated with depression.
- Integumentary: In the literature, children with burns are at risk of furthering or contracting a vitamin D deficiency and its associated side effects due to low sun exposure.
Medical Management
Due to low availability of foods with adequate vitamin D, treatment is largely based on appropriate supplementation and sun exposure.
Supplementation Recommendations:
- Amounts vary depending on cause of deficiency, severity, and physician preference of ramping dosage
- Supplement dosages range from 800 to 1000 IU/d of vitamin D
- Or less than 2000 IU/d to avoid toxicity for those 1 year and old
Dietary Management
Adequate Sources of Intake:
- D2 (ergocalciferol) is found in vegetable sources and oral supplements
- D3 (cholecalciferol) is obtained primarily from skin exposure to ultraviolet B (UVB) radiation in sunlight, ingestion of food sources such as oily fish and variably fortified foods (milk, juices, margarines, yogurts, cereals, and soy), and oral supplements.
Most foods contain between 50 and 200 IU per serving, which varies depending on geographical location and use of the fortification process.
| Food | IUs per Serving* | Percent DV** |
|
Cod liver oil, 1 tablespoon |
1,360 |
340 |
|
Swordfish, cooked, 3 ounces |
566 |
142 |
|
Salmon (sockeye), cooked, 3 ounces |
447 |
112 |
|
Tuna fish, canned in water, drained, 3 ounces |
154 |
39 |
|
Orange juice fortified with vitamin D, 1 cup |
137 |
34 |
|
Milk, nonfat, reduced fat, and whole, vitamin D fortified, 1 cup |
115 – 124 |
29 – 31 |
|
Yogurt, fortified with 20% of the DV of vitamin D, 6 ounces |
80 |
20 |
|
Margarine, fortified, 1 tablespoon |
60 |
15 |
|
Sardines, canned in oil, drained, 2 sardines |
46 |
12 |
|
Liver, beef, cooked, 3 ounces |
42 |
11 |
|
Egg, 1 large (vitamin D found in yolk) |
41 |
10 |
|
Cheese, Swiss, 1 ounce |
6 |
2 |
*IUs = International Units
**DV = Daily Values developed by U.S. Food and Drug Administration
Proper sun exposure
- Cloud coverage can decrease absorption by as much as 50%
- Sun through windows is inadequate-Glass blocks the synthesis process
- Sunscreen may block synthesis if over the entire body
- Get 5 – 30 minutes twice per week between 10AM – 3PM without sunscreen
- Best exposure spots: face, arms, legs, and back
- Tanning beds emit 2-6% UVB (not medically recommended source)
- Limit sun exposure without sunscreen to decrease risk of fatal cancers

