Brain Tumors
Awake Brain SurgeryAwake brain surgery, also called awake craniotomy, is a type of procedure performed on the brain while you are awake and alert. Awake brain surgery is used to treat some brain (neurological) conditions, including some brain tumors or epileptic seizures. It’s the best surgical technique for low-grade gliomas.
If the tumor or the brain lesion is near the parts of the brain that control vision, movement or speech, or anything else important to normal social life, you may need to be awake during surgery. Your surgeon may ask you questions and monitor the activity in your brain as you respond.
Your responses help your surgeon to ensure that he or she treats the correct area of your brain needing surgery. The procedure also lowers the risk of damage to functional areas of your brain that could affect mainly your vision, movement or speech.
Risks
There are risks for awake brain surgery, as for almost all types of brain surgeries:
- Infection or Meningitis
- Movement deficit
- Changes in vision
- Seizures
- Difficulty with speech
- Loss of memory
- Impaired coordination and balance
- Changes in personality or behavior
- Stroke
- Increase fluid in the brain
- Death
Procedure
Before surgery
According to your brain tumor and it’s location, your doctor will first determine if awake brain surgery is the right choice for you. Then, he will explain the benefits and risks of such surgical treatment.
The principle goal of awake brain surgery is to considerably and safely reduce the size of growing brain tumors, which may prolong and improve quality of life.
Before surgery, your neurosurgeon, speech therapist, or neuropsychologist may ask you to identify pictures and words on cards or on a computer so that your answers can be compared during surgery. You will have a complete neuropsychological test before surgery.
During surgery
An anesthesiologist will give you some medication to make you sleepy for the first part of your awake brain surgery. Your neurosurgeon will apply numbing medications to your scalp to ensure your comfort.
Next, your neurosurgeon places your head in a fixed position to keep your head fix and ensure surgical accuracy. Some of your hair may be shaved. Then, your neurosurgeon will remove a part of your skull to reach your brain.
You’ll be sedated and sleepy while part of your skull is removed in the beginning of the surgery, and also when doctors reattach the skull at the end of the surgery. During the surgery, your anesthesiologist will stop administering the sedative medications and allow you to wake up.
After waking up from sedating medications, your neurosurgeon will conduct a first cortical brain mapping, to determine the areas that are directly implicated to your speech, movement, vision, or anything else that can be tested, especially functions related to social interactions.
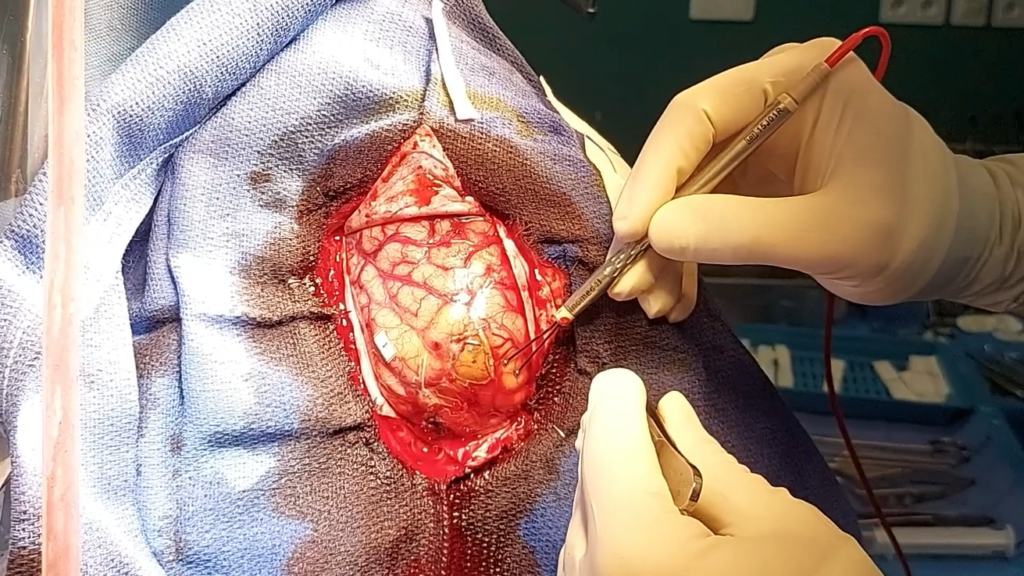
Your neurosurgeon will now attack your brain tumor. while removing the tumor, he will progressively do a subcortical mapping, to detect the long brain pathways that are important to brain functions. He will limit the excision of your tumor just at the level of these pathways.
Brain cortical and subcortical mapping allows your surgeon to safely remove as much of your brain tumor as possible and lower the risks of damaging important body functions.
During surgery, a speech pathologist or neuropsychologist may ask you to do some tasks while your neurosurgeon is stimulating your brain or removing your tumor, like identifying pictures and words on cards or computer that you saw before surgery, or doing some movements with your arm or foot. You are asked also to mention any disturbing sensations, like numbness or flash lights. Your cooperation is crucial for the success of the surgery.
When reaching functional limits, your neurosurgeon will stop the tumor excision and you are again sedated for skull and skin closure.
After surgery
In general, you could have an impressive neurological degradation few hours after surgery, like speech or motor mild to severe disorders. This is in the majority of cases transient, and may signs that your surgeon might do an optimal tumor excision. This is due to inflammatory processes in the surrounding functional brain tissues, that start to exist few minutes to few hours after surgery.
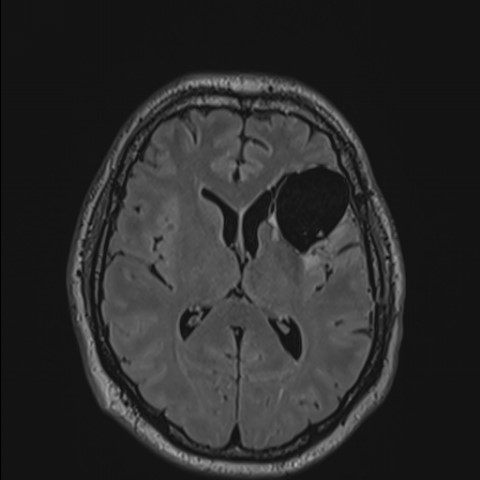
After surgery, your surgeon may request an MRI in the first 24 to 48h to have a first impression on the quality of tumor resection or to assess the residual volume.
You’ll probably be in the intensive care unit for a while after surgery and spend about three to four days in the hospital.
You generally may return to work and normal activities in three months. An intensive speech therapy is very important and has to be done directly after discharge for a quick recovery. You will have a follow-up appointment with your doctor about three months after surgery with a new brain MRI.
In the case of aggressive tumors, you may need extra other treatments, such as radiotherapy or chemotherapy, to help destroy remaining or invisible parts of the tumor, long before the 3 months MRI control (in general 3 to 4 weeks after surgery).
Experience
Dr David has a long experience in the awake brain surgery operating over 100 surgeries in the past 5 years. He does this technique for all cases of low-grade gliomas (in the left as the right side of the brain).

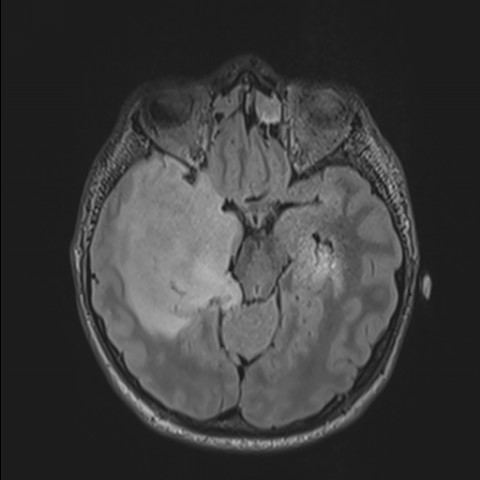
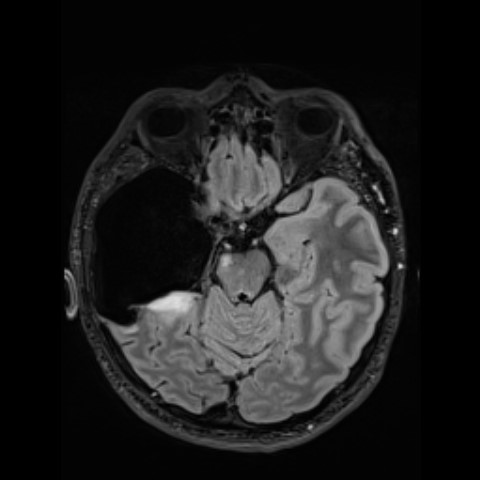
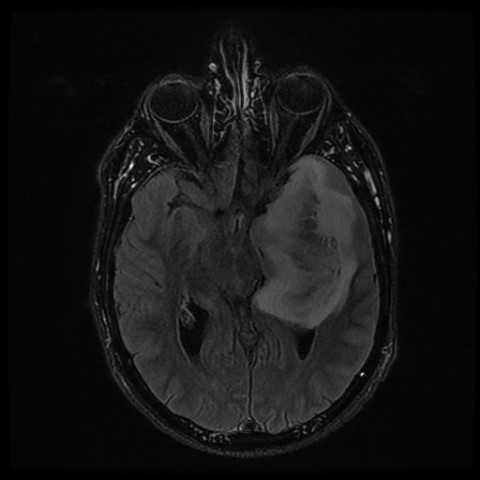
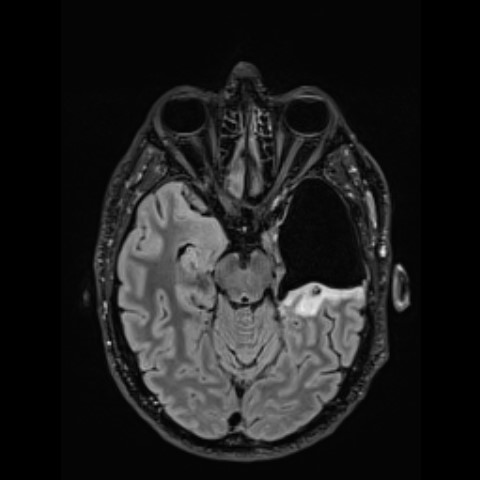
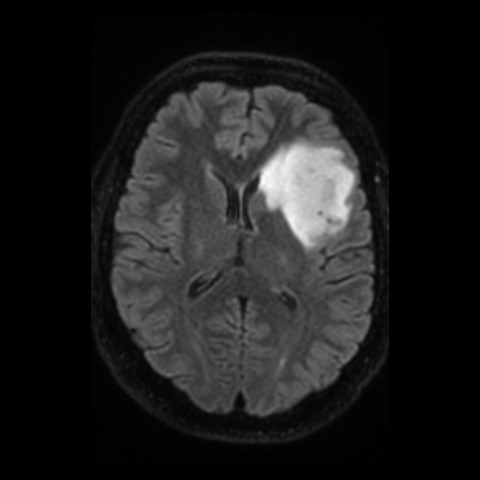
Below you can find some examples of low-grade tumors operated by Dr David, with an excellent clinical outcome. On the left side there is the preoperative MRI and on the right side the postoperative one.